Ketamine Treatment for Obsessive-Compulsive Disorder (OCD)
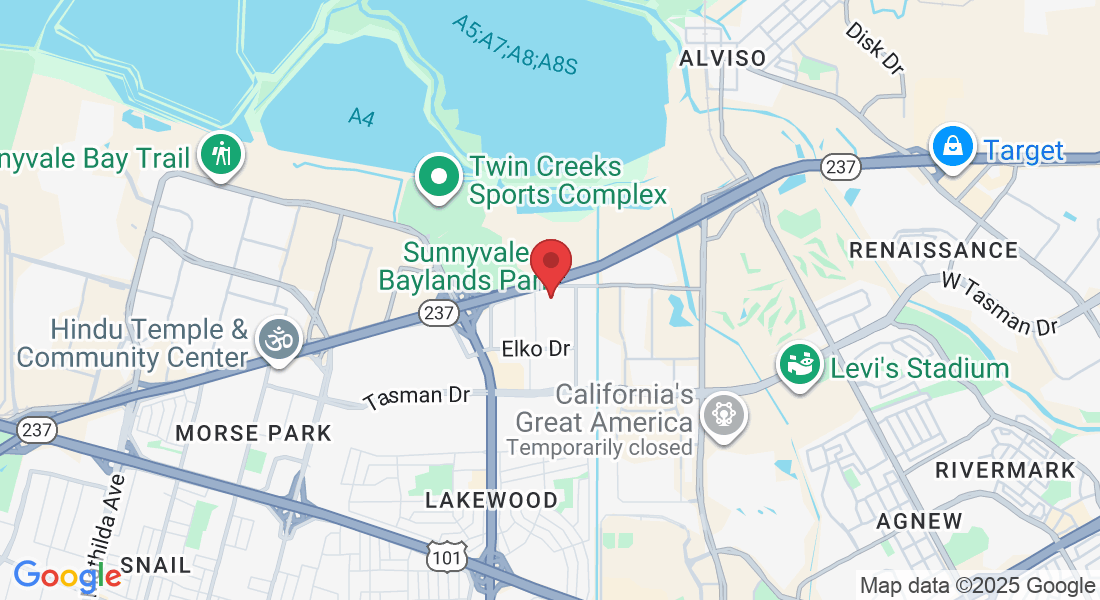
Ketamine Treatment for Obsessive-Compulsive Disorder (OCD) at ACE Medical in Sunnyvale, CA
Living with obsessive-compulsive disorder (OCD) can feel like being trapped in your own mind. Intrusive thoughts, compulsive rituals, and overwhelming anxiety can take over your day, leaving little room for joy, connection, or peace.
If you live in Sunnyvale, CA or nearby communities like Mountain View, Santa Clara, or Cupertino, you may already have tried therapy and medications—and still feel like OCD controls your life.
At ACE Medical, an addiction medicine practice in Sunnyvale, we understand how exhausting and isolating OCD can be. For individuals whose symptoms remain severe despite standard treatments, ketamine therapy has emerged as a potential off-label option that may help reduce intrusive thoughts and anxiety, and increase flexibility in thinking.
While ketamine is not a cure for OCD, early studies suggest it may provide rapid, short-term relief for some people, especially when paired with therapy such as exposure and response prevention (ERP).
Our goal at ACE Medical is to offer this treatment safely, compassionately, and evidence-informed, with a strong focus on addiction risk and long-term recovery.
What is OCD, and how does it affect daily life?
OCD is a chronic mental health condition characterized by:
Obsessions: intrusive, unwanted, distressing thoughts or images
Compulsions: repetitive behaviors or mental rituals performed to relieve anxiety
Common obsessions include fears about contamination, harm, symmetry, sexual or moral concerns, or doubt (“Did I lock the door?”). Compulsions may include washing, checking, repeating, counting, reassurance-seeking, or mental reviewing.
People with OCD often describe feeling:
Stuck in a mental loop
Trapped between fear and ritualizing
Exhausted from constant anxiety
Embarrassed or ashamed of their thoughts
Frustrated that treatment hasn’t worked
First-line treatments for OCD include:
Exposure and Response Prevention (ERP) therapy
SSRIs at higher doses than used for depression
Sometimes antipsychotic augmentation
But even with proper care, as many as 40–60% of patients do not achieve adequate relief from symptoms, leading to treatment-resistant OCD.[1]
What is ketamine treatment for OCD?
Ketamine is an anesthetic that has been used safely for decades. At much lower doses than those used for anesthesia, ketamine has been shown to reduce symptoms of depression, anxiety, and, in some preliminary studies, OCD.[2–6]
For OCD, ketamine is:
Off-label (not FDA-approved specifically for OCD)
Administered in a medical office like ACE Medical—not at home
Given in sub-anesthetic doses, so you remain awake
Used as part of a comprehensive treatment plan, not as a stand-alone solution
Some research suggests that ketamine may temporarily reduce obsessive thoughts and compulsive urges, and may increase the ability to engage in ERP therapy with less distress.
How might ketamine help people with OCD?
OCD is often associated with:
Hyperactivity in cortico-striato-thalamo-cortical (CSTC) circuits
Imbalances in serotonin and glutamate signaling
Reduced cognitive flexibility (feeling “stuck” mentally)
Ketamine acts primarily on the glutamate system, which is critical for learning, habit formation, and emotional regulation. Research suggests ketamine:
Blocks NMDA receptors, altering glutamate transmission
Enhances AMPA receptor activity
Activates pathways like mTOR, which support synaptic growth and neuroplasticity[4–6]
In practical terms, this may help:
Loosen rigid obsessive thought patterns
Reduce the emotional intensity of obsessions
Temporarily interrupt compulsive urges
Increase responsiveness to ERP therapy
Improve mood and anxiety symptoms that worsen OCD[2–6]
Many patients describe ketamine as creating a “mental reset,” giving them a small but meaningful window where OCD feels less controlling.
How effective is ketamine for treatment-resistant depression?
While still emerging, several studies point toward potential benefits:
A randomized controlled trial found that a single IV ketamine infusion significantly reduced OCD symptoms within hours, compared to placebo, though effects faded after about one week.[2]
Open-label studies found that repeated ketamine treatments may produce short-term relief from obsessive thoughts and compulsions in some patients.[3,4]
Some trials suggest that ketamine may help reduce the distress associated with obsessions even when compulsions remain.[3]
Preliminary research on ketamine-assisted psychotherapy indicates possible enhanced effectiveness of ERP when combined with ketamine sessions, due to increased neuroplasticity.[6]
Researchers emphasize that ketamine is not a long-term cure for OCD, but it may be a helpful tool for symptom relief or for improving engagement in therapy.
How does ketamine fit into a long-term OCD treatment plan?
Ketamine works best when combined with:
ERP therapy (the gold standard for OCD)
Medication management (SSRIs, SNRIs, augmentation strategies)
Lifestyle supports (sleep, exercise, mindfulness, structure)
Addiction treatment, if needed
Skills-based therapy, such as ACT (Acceptance & Commitment Therapy)
Our goal is not just temporary relief—it’s helping you reclaim your life from OCD and build long-term resilience.
How does ketamine fit into a broader depression treatment plan?
Ketamine is most effective when combined with:
-Ongoing psychotherapy [6]
-Medication management
-Sleep, nutrition, and lifestyle improvements
-Recovery support if substance use is involved
Our goal is not just rapid improvement—but sustained recovery.
When should I talk to ACE Medical about ketamine for OCD?
Consider a consultation if:
You have severe or treatment-resistant OCD
Standard treatments haven’t provided enough relief
OCD is significantly impacting your daily functioning
You’re interested in a carefully monitored, in-office treatment
You want care from a team that understands both mental health and addiction
A consultation does not commit you to ketamine; it simply helps you understand your options.
Take the First Step Toward Better Health
Whether you're seeking Ketamine treatment for depression, or other mental health or addiction challenges, let ACE Medical be your trusted partner in care.
Experience care that’s personal, proactive, and centered around you.
References:
1. Pallanti S, Quercioli L. Treatment-refractory OCD: definition and therapy challenges.
2. Rodriguez CI et al. Randomized controlled trial of ketamine in OCD.
3. Bloch MH et al. Effects of ketamine infusion on OCD symptoms: open-label studies.
4. Taylor MJ et al. Ketamine and glutamate modulation in OCD treatment.
5. Krystal JH et al. Ketamine’s rapid-acting effects in mood and anxiety disorders.
6. Dore J et al. Ketamine-assisted psychotherapy for OCD: preliminary outcomes.
7. U.S. FDA. Spravato (esketamine) prescribing information and safety updates.
8. Schwenk ES et al. Adverse effects and safety considerations of ketamine use.
Access The Convenient Care You Deserve
Get In Touch
Call, click, or visit — we’re here to make getting care simple & stress-free!
1287 Hammerwood Avenue
Sunnyvale, California 94089
Our Promise to You
Saving lives using evidence-based, ethically-delivered Ketamine Treatment and personalized Addiction Medicine. At ACE Medical, you're not just another patient. You’re a person with a story, and we’re here to support your health, your goals, and your life.
Unlock Your Brain with Ketamine and Medication for Addiction Treatment to help you break free from conditioned responses, limiting beliefs, and emotional patterns that do not empower you.

© 2026 ACE Medical | Accessibility | Terms & Conditions | Privacy Policy | Powered by DoctoGrow